Building the future of rehabilitation and performance
Free Access to The Huddle
Get tips, articles, and news related to rehabilitation and performance delivered to your inbox every week.
The Coaches Club
Two things I love professionally: working with athletes and collaborative learning and creation. Sitting around with a passionate group of professionals discussing, learning, debating... it is one of my favorite things to do.
I have experienced the power of a high-quality community for growth and learning. It changed my career!
To have a place where you can ask questions without being looked down upon, test new ideas, and be at the forefront of learning yet in a structured way.
We built this community to be that place. Join the Coaches Club today!
The Rehab & Performance Lab Podcast
One of my favorite things to do is host a MedBridge live webinar, and the reason for that is we always leave time at the end to answer questions. And those questions are great because they're real world questions. They're questions on topics that maybe are a little more controversial or questions tthe research doesn't specifically answer.
I also love the time that we get to dialog and participate in the real world that way. That's why I'm so excited about the Rehab and Performance Lab podcast. I interview experts who give the information, evidence, and research to answer the practical questions in real time.
This is an opportunity to sit and listen to a conversation behind the scenes with experts. I love doing that. I love learning that way, and I love listening to podcasts. And the great thing about this is you get to earn CEUs with it, too.
Courses for Everyone
Join Phil for engaging courses designed to help you become a better professional.

Optimize Your Career and Prevent Burnout
In healthcare, more than 70% of people are considering some kind of change in their career, whether it is a change in role, setting, hours, or even leaving healthcare altogether. While this signals a major problem, both employers and employees are uncertain how to solve it. Both sides want the same thing: to be happy and engaged in their job. In this course, you will learn the 3 parts of optimizing your career: Part 1 – Identify Your ideal, Part 2 – Work-Life Balance, and Part 3 – Take Your Next Steps.

ACL Reconstruction Rehabilitation Series
ACL reconstruction rehabilitation seems straightforward, yet it is incredibly complex. With so many impairments to work on, how do you prioritize what to address and when to address it? And then how do you know the patient is ready for the next phase of rehab? How do you do this in an efficient manner under the constraints of insurance? Then, when the time comes, how do you know when your patient is ready to return to sport? This course series merges an evidence-based perspective with real-world practice experience and gives you a clear rehabilitation process rather than a rigid protocol to follow.

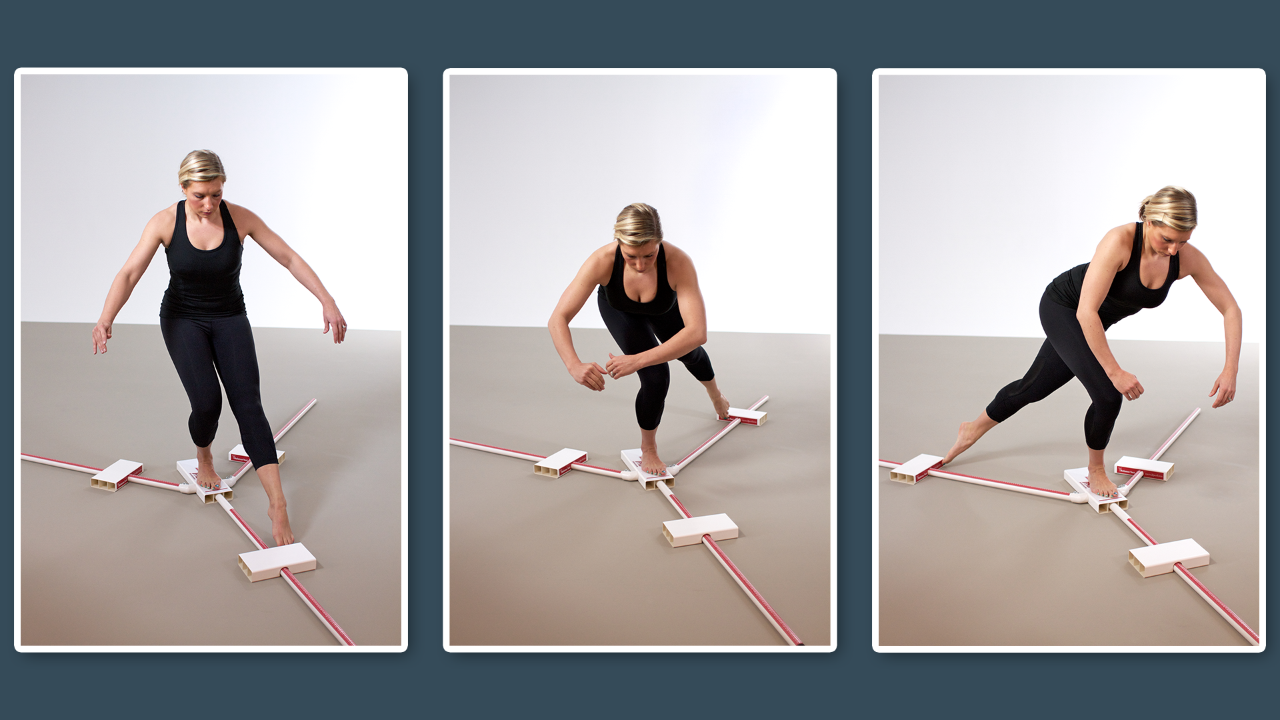
Return to Sport and Discharge Testing
When can I fully return to my activity? It's a simple question with a complex answer. Could you imagine knowing how to make the return-to-activity decision confidently and concretely so the patient, parent, and physician all agree? You can dramatically impact your patients' health and reduce reinjury rates by making evidence-based discharge and return-to-sport decisions. There is no guesswork; there is a data-driven decision. This course will lay the foundation to help you develop a scientific decision-making process, select evidence-based tests, and apply them to patient care.

Meet Phil!
I'm a physical therapist, athletic trainer, strength and conditioning coach, and Professor in the Doctor of Physical Therapy & PhD Programs at the University of Evansville.
As a performance systems consultant with all major professional sports and the military, my passion is teaching athletes how to elevate their game to the next level.
Additionally, I help rehabilitation and performance professionals maximize their client’s physical potential by teaching them how to live a fully engaged life, systematic thinking, testing and interventions so that they and their clients can remain healthy, fit, and well.
More About Me
Dan Marr
Director of NHL Central Scouting
"Dr. Plisky’s expertise and proficiency with the Y Balance Test has become an integral part of the NHL Combine screening procedures. His level of professionalism in administering large group screening is unparalleled and provides vital insights on athletes. His presence in overseeing the testing instills confidence in the process and results with both athletes and strength and conditioning specialists alike."

Jon Torine
Former NFL Head Strength & Conditioning Coach, World Champion Indianapolis Colts
"In life there are people that you know you can go to that can solve problems, offer wisdom, expertise, and make the complicated simple. Through my 25 years of coaching, 17 in the NFL, consulting and implementing systems across youth, college and pro sports I’ve been fortunate to have a few of those people. I am honored to say that Phil Plisky is one of those guys. Phil has an easy to understand brilliance and way of working with people that both puts them at ease and challenges you to look at multiple perspectives. When it comes to testing, assessments, return to play, injury reduction, and improving athletes health and efficiency there are few I trust as much as Phil."

Teena Murray
Sr. VP of Integrated Performance, Pittsburgh Penguins
“Phil brings a unique approach to the table. As an athletic trainer, physical therapist and strength coach, he is able to connect across the spectrum of injury, prevention, and performance, speaking the language needed to engage, educate and empower all members of the group/team. I have leaned on Phil many times in many scenarios, and trust his ability to make an impact.”
Looking for Return to Sport Criteria?

Return to Sport Checklist
Spine
Back or neck injury, make confident return to sport decisions

Return to Sport Checklist
Upper Body
This checklist includes the complexities that an upper extremity injury brings including overhead athlete
You aren't subscribed to MedBridge?
Get the best price using promo code "PLISKY". View all of Phil's courses here!
Do you have a clinical or career question?
My passion is helping people be their best, so If you have any questions, or comments, simply fill out the form below and I’ll get back to you as soon as possible!