How do you know if someone is ready to return to work or sport after injury?
How would you respond if someone asked, “How much would you bet that your patient or client is ready to go back to sport, work, or daily activity without increased risk of injury?” We may never be completely confident and it won’t be a sure bet. But, how do you determine a patient’s readiness? If previous injury is a risk factor for future injury, are we actually sending people back at their optimal level? We had the same questions.
In the last post I discussed the research regarding how managing the number of risk factors someone has may be the key to optimizing our outcomes with rehabilitation and performance. Start by reading that post or watching that video first because we are now going to discuss those risk factors when it comes to rehabilitation and discharge.
To recap, we tested 1466 soldiers to identify the most robust risk factors for injury. The risk factors were important, but even more so the number of those risk factors when looking at the relationship to future injury. The more risk factors someone had, the more likely to get injured. Thus, our goal in performance or rehabilitation should always be to test and determine the risk factors in order to work on reducing them.
Time and time again, previous injury, length of time loss, and perceived recovery come out as risk factors. So what can we do after someone gets hurt to reduce this?
Here is what we did in the second major study. We wanted to see what soldiers looked like after an injury when they were cleared for full duty. Secondly, we prospectively followed these folks out for a year to see if the same risk factors predicted re-injury and if the cut points remained the same. We added some additional tests like the Selective Functional Movement Assessment (SFMA) top tier movements, weighted shuttle run, 75% bodyweight carry, etc.
Here are two of the research questions we asked (Here is the Free Full Text Research Paper):
What percent of those cleared for full duty had pain with the simple movements in the Top Tier SFMA?
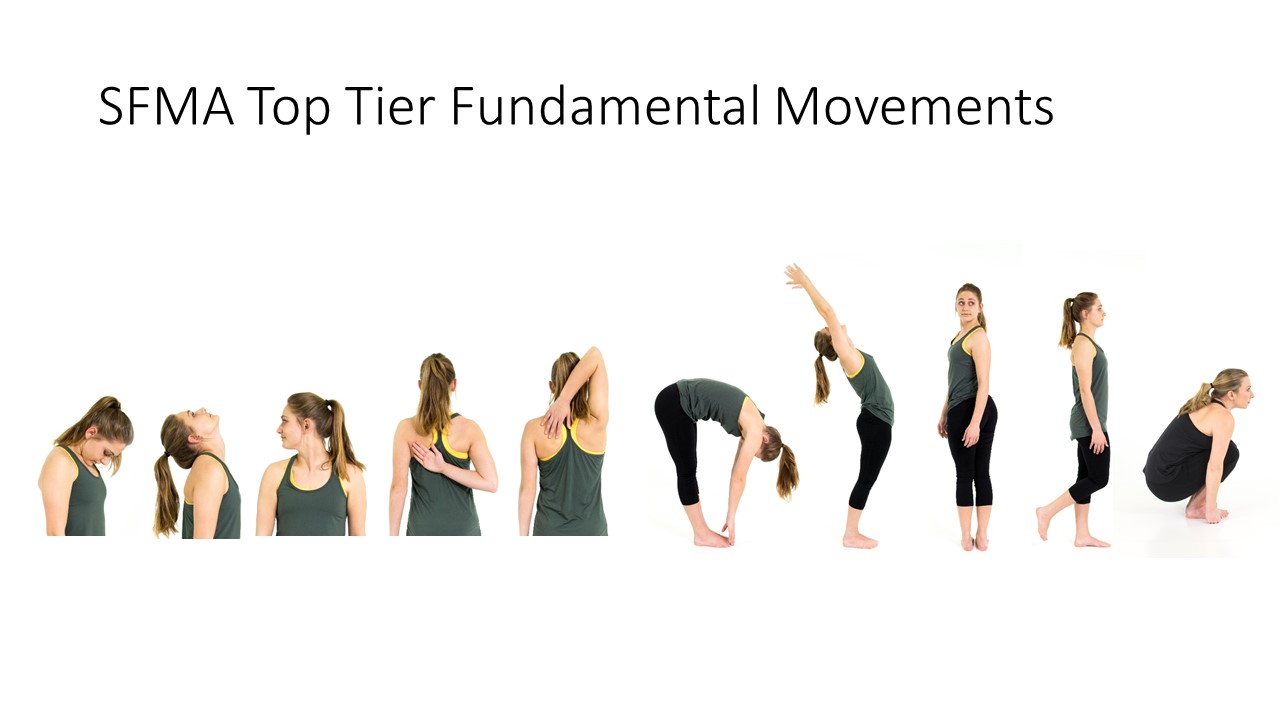
The SFMA is a movement based diagnostic system and provides healthcare professionals with an efficient and systematic tool to reach a comprehensive movement diagnosis.
The entry point into the system is the Top Tier tests — 7 basic movement patterns graded as Functional and Non-painful (FN), Functional Painful (FP), Dysfunctional Non-painful (DN), and Dysfunctional Painful (DP). If a Top Tier test does not pass the FN grade, then that specific movement must go to a breakout pattern to find the true cause of dysfunction.
We found that 44% had pain on the top tier Selective Functional Movement Assessment!!!!!!! Let that sink in for just a moment…44% of soldiers had pain with a basic movement like touching their toes or squatting……after they had been released as “good to go” from their injury.
What percent of those cleared for full duty had 5 or more risk factors?
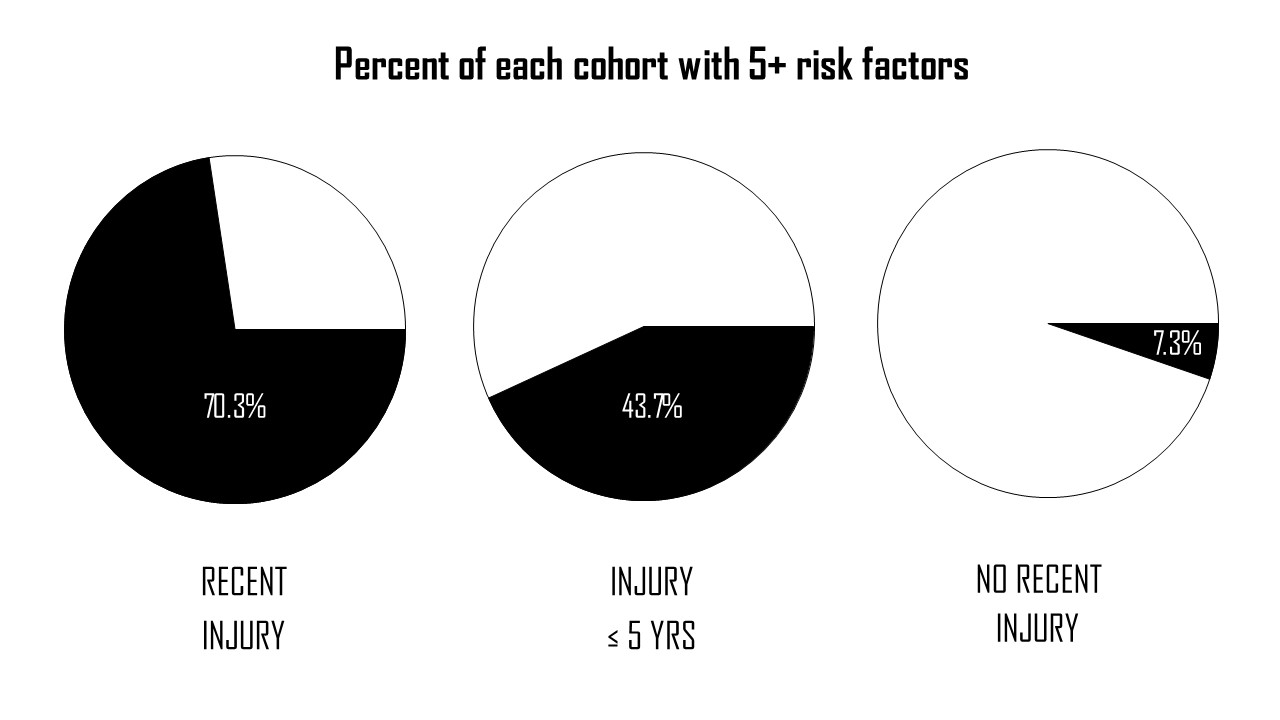
Remember, having 5 or more risk factors substantially increased your likelihood of getting injured (see previous post).
70% of those cleared for duty had 5 or more risk factors (to be fair, they already possessed 2 of the risk factors of profile time and previous injury). Compare that to the 40% who had 5 or more risk factors in the previous study and had an injury in the last 5 years. On the other hand, those who had not sustained an injury in the past 5 years, only 7% had 5 or more risk factors.
To summarize, we found 70% of those cleared for duty, who were classified as ready, still had 5 or more risk factors for injury. That difference cannot be ignored.
Check out this great infographic developed by @DrMariahDPT. The quote at the bottom says it all. @danrhon @dteyhen pic.twitter.com/xlEzBB9MJ2
— Phil Plisky (@PhilPlisky) March 24, 2022
Now, what should we do with these findings?
We may be managing the local problem (knee, back, etc.) in rehabilitation, but we may not be managing risk factors. We need to think about rehabilitation differently. Certainly, let’s continue to get people out of pain, but let’s look at creating a standard operating procedure for testing and mitigating risk factors as part of our rehabilitation plan.
1. TEST RISK FACTORS
First, let’s test for the risk factors. Which ones should we test and what should they be? Right now, until we have the results of this most recent study analyzed we should be testing:
Risk Factors From Survey Data
-
- Age > 26
- Sex: Female
- Prior Injury
- Perceived Recovery
- Length of Profile
- Army Run ≥ 15.3 min
Risk Factors From Physical Testing
-
- DF Asymmetry ≥ 4.5°
- YBT-LQ: Anterior Reach ≤ 72% Limb Length
- YBT-UQ: Superolateral Reach ≤ 80.1% Limb Length
- YBT-UQ: Inferolateral Reach Asymmetry ≥ 7.75
- Pain present with Movement
For example, after an ankle sprain we may fix the person’s dorsiflexion range of motion and restore their ankle strength and lower extremity balance, but if they have hip pain with a squat below 90 degrees, that is a risk factor we need to fix even if wasn’t related to the original injury.
2. USE/CHANGE DISCHARGE CRITERIA
Let’s continue rehabilitation until that person has reduced their number of risk factors rather than only rehabilitating the primary problem. This should go a long way to reducing musculoskeletal pain being one of the most costly diagnoses for our health care system and one of the greatest factors impacting our military readiness.
In the next post, we will discuss another study from our research that may help us get buy in for patients and athletes on reducing risk factors. Because, quite frankly, very few people care about risk factors. Spoiler alert, people do care about performance and possessing risk factors has an influence on performance!
As a sneak peak, here are the prospective injury risk results from this study
Developing a model to predict re-injury after being cleared to return to full military duty after MSK injury #WCSPT2022 #Infographic @DrGSBullock @MilitaryHealth pic.twitter.com/WsXK2d4YJh
— Dan Rhon (@danrhon) August 26, 2022
Rhon DI, Teyhen DS, Kiesel K, Greenlee TA, Shaffer SW, Goffar SL, Plisky PJ. Does Recency of Musculoskeletal Injury Strengthen Association between Past Injury History and Future Injury Risk? Podium, APTA CSM Annual Conference, Denver, CO. February 2020
Rhon DI, Teyhen DS, Kiesel K, Shaffer SW, Goffar SL, Greenlee TA, Plisky PJ. Recovery, Rehabilitation, and Return to Full Duty in a Military Population After a Recent Injury: Differences Between Lower-Extremity and Spine Injuries. Arthrosc Sports Med Rehabil. 2022 Jan 28;4(1):e17-e27. doi: 10.1016/j.asmr.2021.09.028. PMID: 35141533; PMCID: PMC8811499.










